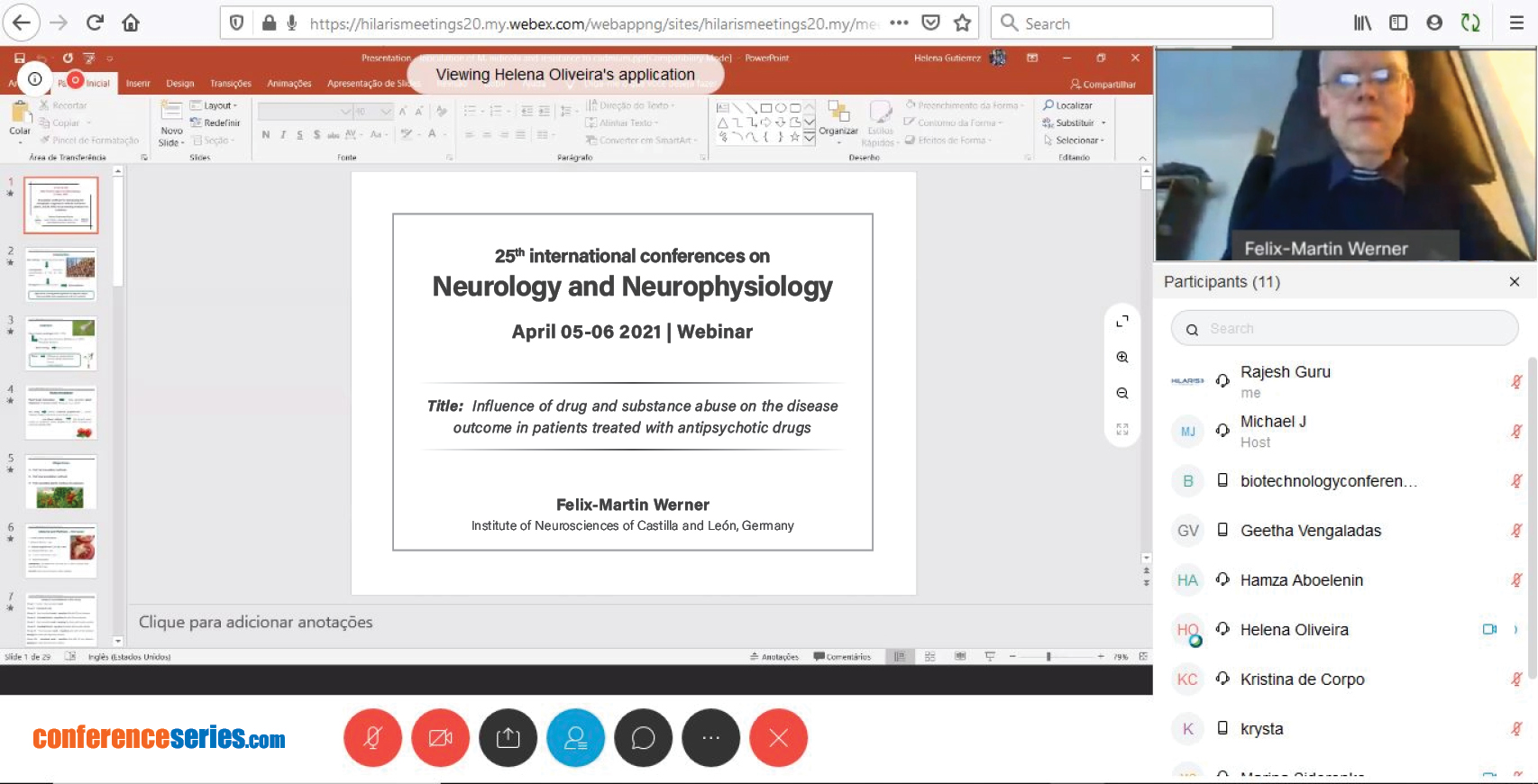
Felix-Martin Werner
Institute of Neurosciences of Castilla and León, Germany
Title: Influence of drug and substance abuse on the disease outcome in patients treated with antipsychotic drugs
Biography
Biography: Felix-Martin Werner
Abstract
Schizophrenia is a chronic mental and disabling disease, which has a heritability of 50 %. Some susceptibility genes have been discovered. In schizophrenic patients, second-generation antipsychotic drugs are administered, but a long term therapeutic effect is not secure. Some schizophrenic patients show treatment-resistant forms of psychosis. In some cases, the SGA clozapine shows a therapeutic effect after some months later. Schizophrenic patients tend to show a reduced adherence to the pharmacotherapy and to consume substances such as alcohol, nicotine and, in some cases, drugs such as cannabis and amphetamines. Some retrospective studies reported that the reduced adherence to the antipsychotic pharmacotherapy was combined with the consumption of substances. Substance such as alcolol and nicotine can worsen psychotic symptoms. Cannabis has two compounds, e.g. tetrahydrocannabinol, which is psychotomimetic, and cannabidiol, which is antipsychotic. Amphetamines can as well worsen psychotic symptoms. Psychoeducation, for example the mindful-based form helps to improve the patients’ compliance and to reduce the substance abuse. The long-acting injectable forms of antipsychotic drugs can make sure the regular administration of these drugs. Patients taking regularly their antipsychotic drug have a better social functioning and a better clinical outcome. In order to reduce the substance abuse, additional drugs such as vanecriline, a nAch agonist, and rimonabant, a CB1 receptor antagonist can be administered.